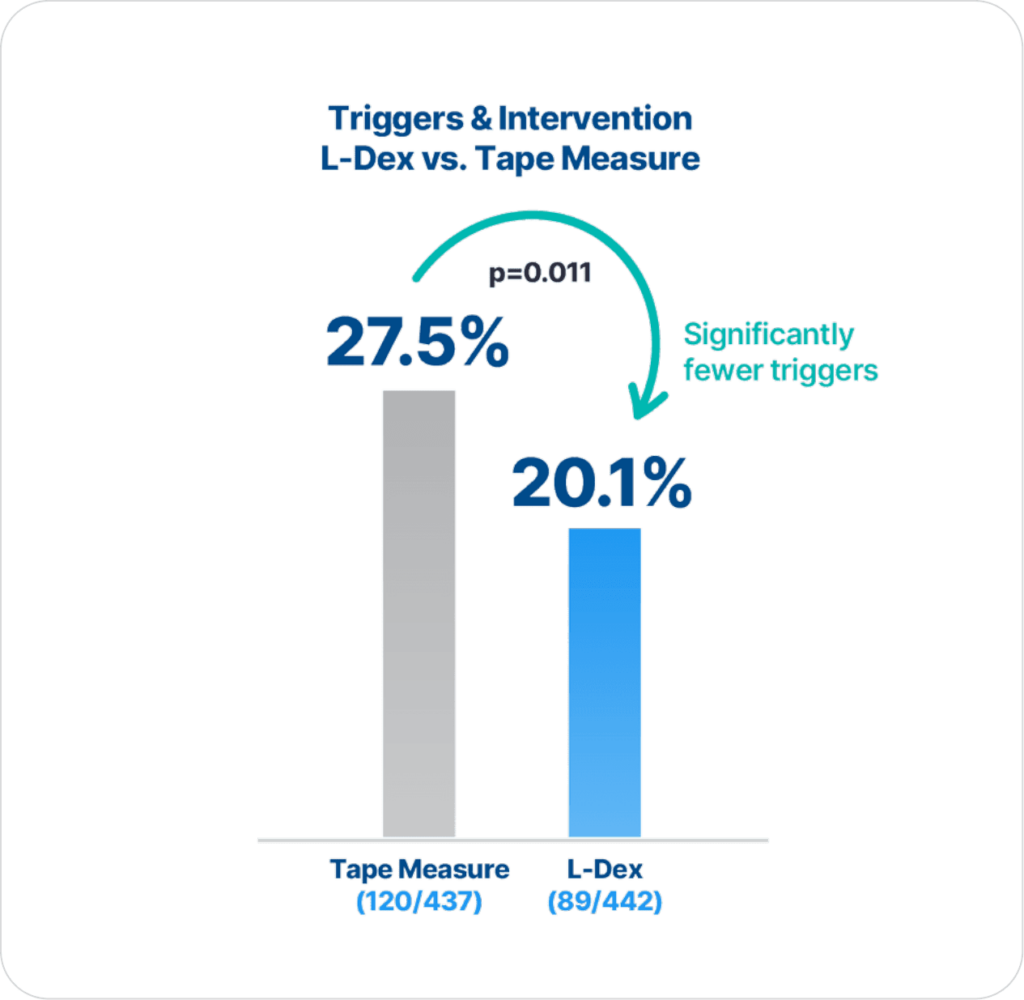
ImpediMed’s BIS technology is more precise and reliable than tape measure in detecting lymphedema (LE), as there are statistically significantly fewer triggers and interventions for those assessed with BIS compared to tape measure (p=0.011)2.
Extensive clinical evidence shows that using ImpediMed’s bioimpedance spectroscopy (BIS) technology for early detection and intervention reduces the impact of chronic lymphedema on breast cancer patients.
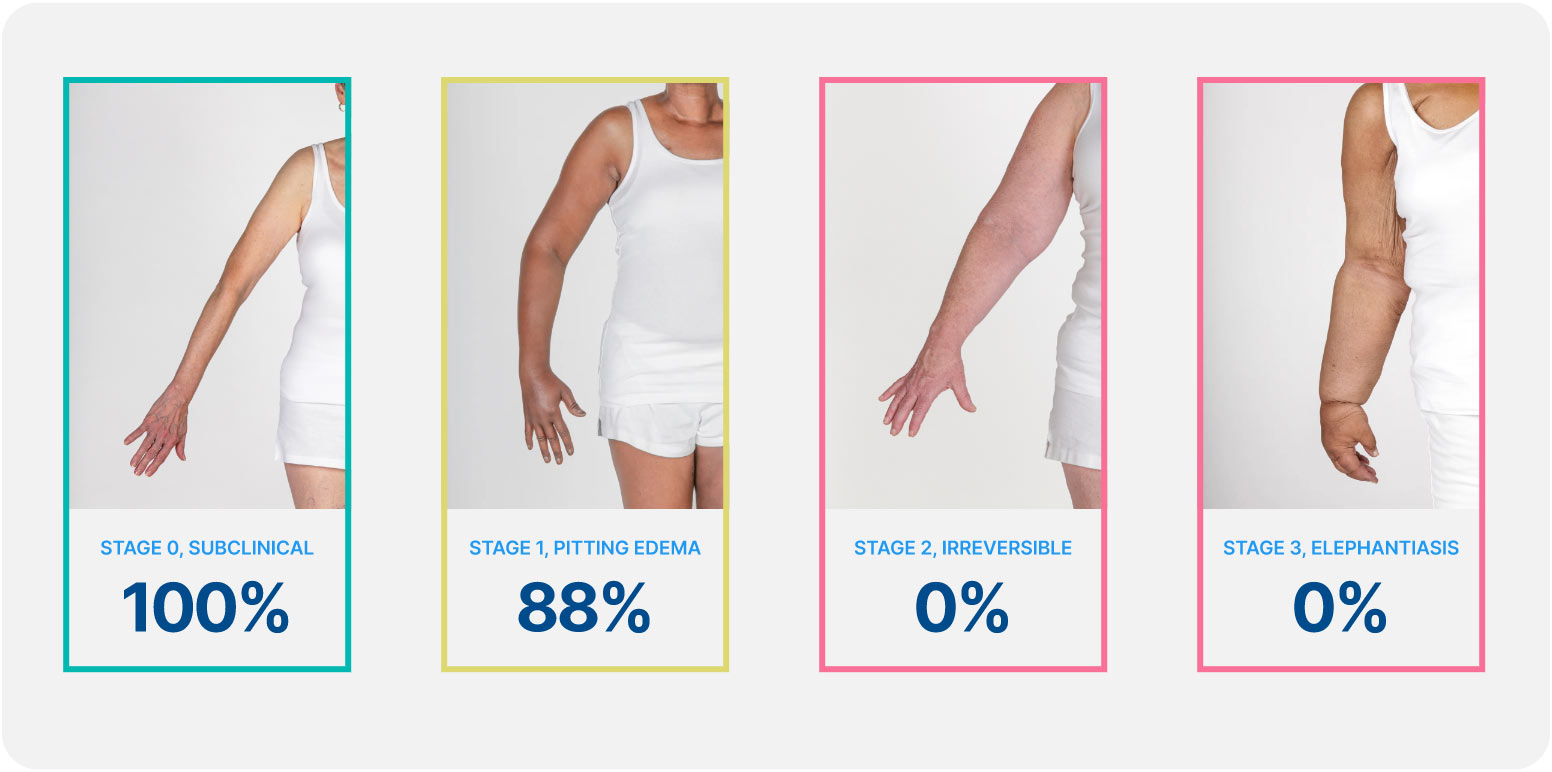
Lymphedema develops in stages, and a university of Kansas study found that when lymphedema is detected at stage 0 or stage 1 it is reversible, but in stages 2 and 3 it is not. These findings demonstrate how early conservative intervention and prospective monitoring with BIS can significantly lower rates of BCRL and persistent BCRL (pBCRL).¹
The PREVENT Trial involved 10 centers across the US and Australia and was the largest randomized controlled trial (RCT) to assess lymphedema prevention in breast cancer patients.
To our knowledge, this is the first prospective study of patients who underwent ALND for breast cancer in which BIS technology was used to detect LE and evaluate the benefits of early diagnosis and treatment interventions objectively. We demonstrated that periodic monitoring of women at high risk for LE, with BIS technology, allowed detection of subclinical LE and timely intervention for treatment, resulting in a reduction of clinical LE from 36.4% to 4.4%. Future studies will determine whether this translates into reduced total health care costs and improved quality of life for patients with breast cancer.
Soran, A., et al., The importance of detection of subclinical lymphedema for the prevention of breast cancer-related clinical lymphedema after axillary lymph node dissection; a prospective observational study. Lymphat Res Biol, 2014. 12(4): p. 289-94
Giving that all the women who were treated for breast cancer are at life-time risk for lymphedema, using assessment methods that can accurately identify true lymphedema cases among at-risk breast cancer survivors is of the ultimate importance for clinical practice. Perhaps, the most important contribution of our study was that it has provided evidence that, using a cutoff point of L-Dex ratio of >+7.1, cross-sectional assessment of BIA was able to discriminate at-risk breast cancer survivors and those with lymphedema.
Fu, M.R., et al., L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology, 2013. 46(2): p. 85-96,
Economic analysis demonstrating that BIS utilization would lead to a cost savings which is magnified when considering sequelae of BCRL.
Over 1 year, BIS-aided assessment of lymphedema for patients following treatment for BC results in cost savings, even without considering potential cost savings associated with averted downstream sequelae.
Bilir, S.P., M.P. DeKoven, and J. Munakata, Economic benefits of BIS-aided assessment of post-BC lymphedema in the United States. Am J Manag Care, 2012. 18(5): p. 234-41.
Early intervention may reduce the need for intensive rehabilitation and may be cost saving. This perspective article compares a prospective surveillance model with a traditional model of impairment-based care and examines direct treatment costs associated with
each program.
The prospective surveillance model includes the cost of screening all women plus the cost of intervention for early-stage BCRL. The TM group comprised women referred for BCRL treatment using a traditional model of referral based on late-stage lymphedema. The
traditional model cost includes the direct cost of treating patients with advancedstage lymphedema. The cost to manage early-stage BCRL per patient per year using a prospective surveillance model is $636.19. The cost to manage late-stage BCRL per patient per year using a traditional model is $3,124.92. The prospective surveillance model is emerging as the standard of care in breast cancer treatment and is a potential cost-saving mechanism for BCRL treatment.
Stout, N.L., et al., Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther, 2012. 92(1): p. 152-63
The choice of the mean + 3 SD as the criterion value may be questioned as being too conservative compared to a criterion of the mean + 2 SD more common in diagnostic testing. This threshold value was originally proposed by Cornish et al. but without supporting explanation for its choice. Its use in the present study was based upon this historical precedent.
Ward, L., et al., Confirmation of the reference impedance ratios used for assessment of breast cancer-related lymphedema by bioelectrical impedance spectroscopy. Lymphatic Research and Biology, 2011. 9(1): p. 47-51
Study of 172 healthy females indicates that impedance ratio thresholds are consistent with those previously identified.
In summary, new criterion thresholds for the assessment of BCRL by BIS have been determined. Although statistically different to the established reference values, the magnitude of the difference is sufficiently small to be of no practical clinical consequence. It is concluded that, in accord with the observations of Ridner et al., the present reference thresholds may be used with confidence as markers for lymphedema.
Ward, L., et al., Confirmation of the reference impedance ratios used for assessment of breast cancer-related lymphedema by bioelectrical impedance spectroscopy. Lymphatic Research and Biology, 2011. 9(1): p. 47-51.
The impedance ratio thresholds for lymphedema of the legs have been established, opening the way for BIS to become established clinically for the early detection and assessment of lower limb lymphedema.
Ward, L., et al., Reference ranges for assessment of unilateral lymphedema in legs by bioelectrical impedance spectroscopy. Lymphatic Research and Biology, 2011. 9(1): p. 43-46
BIS offers a good possibility to monitor the water content of a person. This can be used in monitoring decompensated CHF patients. Since most patients with acute heart failure suffer not only from lung edema, but also from edema in limbs a combination of segmental and whole body BIS measurements offers the best options to supervise the course of diseases. In this paper, both BIS measurements show a strong correlation with the water balance and weight loss.
Beckmann, L., et al., Monitoring of body fluid in patients with chronic heart failure using Bioimpedance-Spectroscopy. IFMBE Proceedings 25/VII, 2009. 25: p. 532-535.
Claims study of 1,877 patients for 2 years after the start of cancer treatment. 10% of patients developed lymphedema with ALND and chemotherapy associated with development. Higher medical costs associated with BCRL diagnosis ($23, 167 vs. $14,877) with higher rates of cellulitis/lymphangitis noted.
Although the use of claims data may underestimate the true incidence of lymphedema, women with BCRL had a greater risk of infections and incurred higher medical costs. The substantial costs documented here suggest that further efforts should be made to elucidate reduction and prevention strategies for BCRL.
Shih, Y.C., et al., Incidence, Treatment Costs, and Complications of Lymphedema After Breast Cancer Among Women of Working Age: A 2-Year Follow-Up Study. J Clin Oncol, 2009.